Is depression a problem affecting the brain as an organ, a disorder of thoughts and how we use the mind, or could it stem from a broader issue in the body? From a lecture by Daniel Nettle at the Evolutionary Psychiatry Group of the Royal College of Psychiatrists, presented by Riyad Abed.
Nettle begins by discussing the complexities of defining depression within neuroscience and psychology. He highlights the rising prevalence of depression and ongoing challenges in treating it effectively. A key point is that research and pharmaceutical advancements have not significantly improved outcomes in reducing depression symptoms or prevalence. The scientific debate persists on whether depression is primarily a brain disorder or a mental one—centered on thoughts—affecting treatment approaches.
While core symptoms like low mood and loss of interest are primarily psychological, other symptoms, such as changes in appetite and sleep, blur the line between mental states and physical conditions. There’s an overlap between physical symptoms and mental states; for instance, suicidal thoughts are central to depression, but symptoms also manifest physically. Depression can lead to diverse physical symptoms like insomnia, loss of appetite, and energy depletion, showing a complex interplay between mind and body.
If depression is a mental illness, why do neuroscientific studies lack consistency in identifying brain activity differences in depression? Despite extensive brain imaging research, no consistent neural targets for depression have been pinpointed. For example, reduced hippocampal volume is observed in depressed patients, but its significance and cause remain unclear. Conversely, immune system differences suggest significant links to depression beyond brain activity. Studies show elevated immune markers, like interleukin and C-reactive protein, in depressed individuals. Depression is also linked to physical conditions like type 2 diabetes and metabolic syndrome, indicating a complex interaction between metabolic health and mental illness. Research notes generally higher body temperatures and consistent immune markers in depressed individuals

A study on predicting depression within a symptom network highlights the strong role of physical factors in prediction [2]
Even with medications, while current antidepressants generally outperform placebos, they lack long-term efficacy. However, drugs affecting bodily immune activity show effects, including alleviating depression. Non-steroidal anti-inflammatory drugs like ibuprofen and cytokine inhibitors demonstrate notable effectiveness in reducing depression by targeting the immune system.
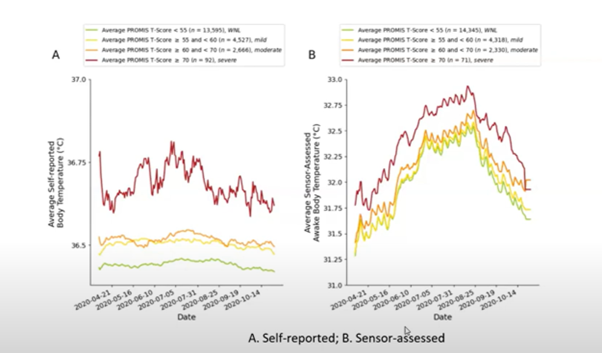
A study shows elevated body temperature in depressed individuals, suggesting a potential link
Depression may be a metabolic condition influenced by immune responses, not just a cognitive issue. Depression symptoms resemble sickness behavior in animals, involving energy conservation and risk avoidance. Current assessment methods often overlook metabolic and inflammatory factors in diagnosing depression. Exploring metabolic and inflammatory changes could expand treatment options and challenge neuroscience’s focus on depression. The interplay between physical and mental health suggests lifestyle changes impact depression, possibly tied to modern life. Chronic stress in modern society may lead to prolonged sickness behavior, contributing to depression’s prevalence. Modern life’s unique pressures differ from those of the past.
In conclusion, this summary doesn’t replace the information-rich lecture. Attributing depression to physical factors like immunity remains speculative and not yet a scientific theory.
[1] Müller, Veronika I., et al. “Altered brain activity in unipolar depression revisited: meta-analyses of neuroimaging studies.” JAMA psychiatry 74.1 (2017): 47-55.
[2] Boschloo, Lynn, et al. “A prospective study on how symptoms in a network predict the onset of depression.” Psychotherapy and psychosomatics 85.3 (2016): 183-184.


0 Comments